Ultimate Guide to Patient Feedback Channels

Key Takeaways
Ultimate Guide to Patient Feedback Channels
Patient feedback channels help healthcare companies understand patient needs, experiences, and satisfaction. These channels include surveys, interviews, social media, and patient portals. Insights from feedback can improve care, boost patient retention, and support regulatory approvals. Companies that act on feedback often see higher revenue growth and better outcomes.
Key Takeaways:
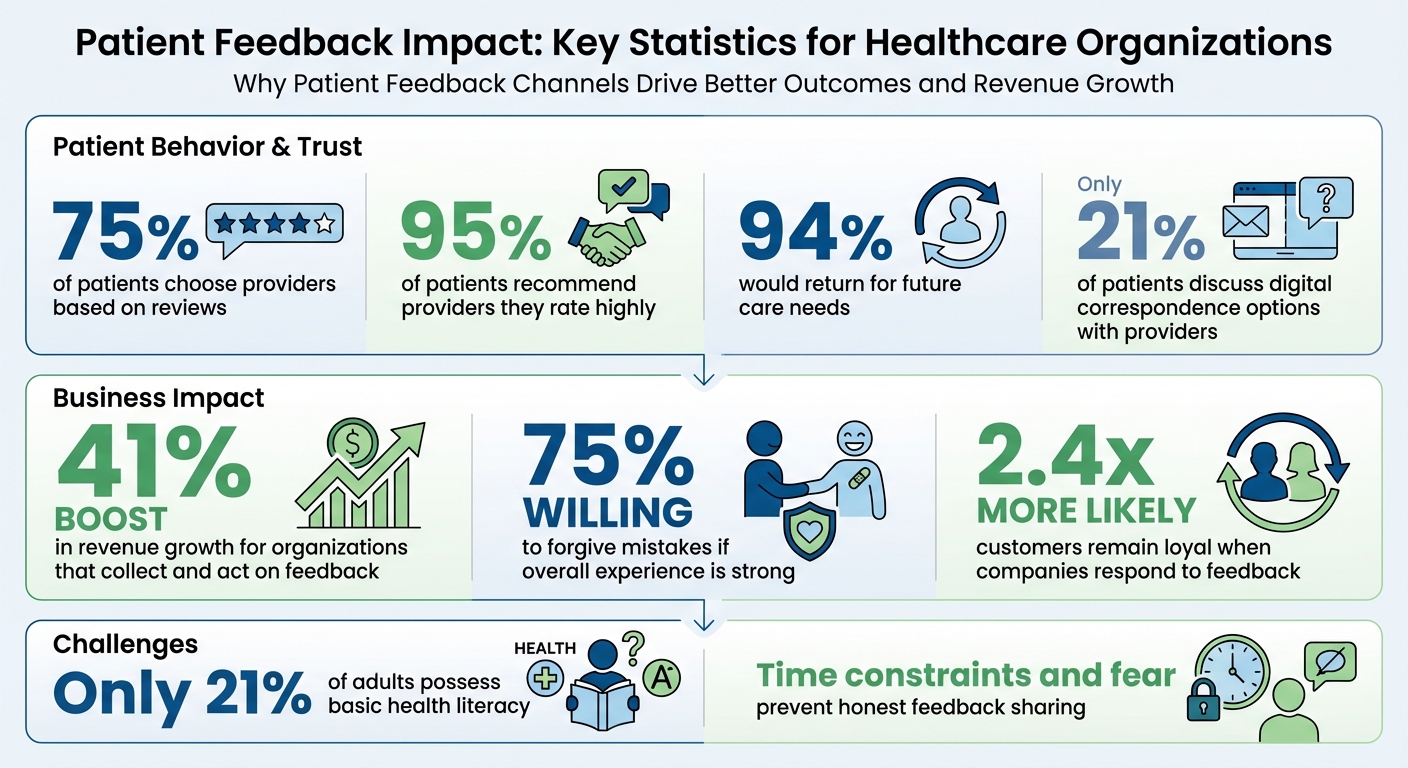
- Why Feedback Matters: 75% of patients choose providers based on reviews, and 95% recommend providers they rate highly.
- Types of Channels: Digital surveys, SMS, interviews, focus groups, and AI tools.
- Challenges: Patients may hesitate to share honest feedback due to fear, time constraints, or complex forms.
- Solutions: Build trust, simplify communication, and ensure data security.
- Actionable Steps: Automate feedback collection, analyze insights, and act on patient suggestions.
Patient feedback isn't just data - it's a tool to improve care and outcomes while strengthening trust with patients.
Patient Feedback Impact: Key Statistics for Healthcare Organizations
7 Easy Ways to Collect Real Patient Feedback
sbb-itb-8f61039
What Are Patient Feedback Channels?
Patient feedback channels are organized methods designed to capture the "Voice of the Patient" (VoP). These channels help healthcare organizations understand patient needs, emotions, and satisfaction levels throughout their care journey - from the initial search for treatment options to long-term adherence and outcomes.
By gathering this data, organizations can pinpoint service gaps and identify areas where improvements in people, processes, or technology are needed to deliver more personalized care experiences. For pharmaceutical and med-tech companies, these insights are invaluable. They reveal patient sentiment during treatment journeys, helping improve adherence and clinical outcomes. Many advanced systems now collect real-time feedback by automatically triggering requests at key moments in the care process.
"The voice of the patient helps the organizations in the industry understand how patient needs, emotions, and levels of satisfaction change throughout the healthcare experience." – Qualtrics
The rise of omnichannel feedback collection has transformed how companies gather data. Now, feedback comes from various sources, including text messages, emails, in-app prompts, and social media. Additionally, tools powered by AI and natural language processing can analyze unsolicited feedback from call center transcripts, chat logs, and social media posts. This shift turns feedback into an active "system of action", where negative feedback can trigger immediate efforts to resolve issues.
Types of Patient Feedback Channels
Patient feedback comes in many forms, each suited to specific needs:
- Digital surveys: Scalable and easy to analyze, often used after appointments.
- SMS prompts: Effective for mobile users due to high open rates.
- Patient portals: Provide ongoing feedback tied to operational data.
- Direct interviews: Offer deep insights into complex conditions.
- IVR systems: Capture fresh data from call center or HUB interactions.
- Focus groups: Gather diverse perspectives, especially useful in early trial design.
However, there’s a communication gap to address. Only 21% of patients report discussing digital correspondence options with their healthcare providers, leaving many to rely on phone channels instead. This highlights the need for multiple feedback methods that align with patients’ preferences and comfort levels.
Why Pharma and Med-Tech Companies Need Patient Feedback
Patient feedback is more than just a tool for improvement - it directly impacts both business and clinical success. Organizations that actively collect and act on feedback see a 41% boost in revenue growth. Moreover, 95% of patients who rate their care as "very good" are likely to recommend the provider, and 94% would return for future care needs.
Feedback also helps uncover barriers in processes, policies, and technologies that might hinder effective treatment. For example, the inhaled insulin product Exubera was pulled from the market in 2007 after generating only $12 million in sales over nine months - far short of its $2 billion target. The failure was largely due to a lack of patient input during development, as users found the device cumbersome and the instructions unclear. This case underscores the importance of incorporating patient feedback early to avoid costly missteps.
Real-time feedback systems add another layer of value by enabling "service recovery." They allow organizations to address negative experiences immediately, reducing patient churn and improving long-term adherence. Beyond resolving issues, feedback also supports regulatory decisions, aiding benefit-risk assessments and the development of clinical outcome assessments (COAs). The FDA’s emphasis on Patient-Focused Drug Development (PFDD) highlights the growing importance of systematic patient feedback in gaining regulatory approvals.
One standout example is the iConquerMS Multiple Sclerosis Patient-Powered Research Network. By enlisting trusted MS patient bloggers to promote the network, they significantly boosted enrollment. This shows that feedback channels aren’t just about data collection - they also build trust and foster communities that lead to better patient outcomes.
How to Set Up Patient Feedback Systems
Gathering patient insights is essential, but it’s not enough to simply collect feedback - you need a system that integrates collection, analysis, and action. A well-designed feedback system ensures you’re not just listening but also responding in meaningful ways. Start by setting clear objectives, using research and expert input to craft focused questions.
Collection: Tools and Channels
To reach a broad audience, use multiple feedback channels. While digital tools are popular, 21% of patients still prefer phone calls.
Pharma-specific channels offer tailored solutions for different scenarios. For example, generic survey links are ideal for clinical trials where you don’t have direct patient contact information. These can be embedded in patient portals or shared through marketing materials. Interactive Voice Response (IVR) systems are great for capturing immediate feedback after phone interactions with case managers or HUB services. Email surveys, on the other hand, allow for more in-depth questions and can be linked with operational data, such as tracking satisfaction by case manager.
A real-world example: In September 2024, a pharmaceutical company specializing in rare diseases launched an IVR survey program during a new product rollout. Patients were directed to a phone survey immediately after speaking with case managers, enabling the company to gather satisfaction data within a month. This feedback helped coach case managers and improve interactions with their small, specialized patient base.
Automation is key to ensuring unbiased data. When case managers manually decide whether to transfer patients to a survey, they might avoid doing so after negative interactions - a behavior known as "agent bias", which skews results.
"By automating your IVR feedback program, you're controlling for a major variable that could adversely impact the integrity of your data: case manager or agent bias." – PeopleMetrics
Question design is just as critical as choosing the right channels. Avoid combining multiple questions into one (e.g., “How embarrassed and self-conscious have you been?”). Instead, separate them for clarity. Use simple, clear language that accommodates all health literacy levels, and always pilot test your surveys with a small sample of your target audience to catch potential issues before a full rollout.
Analysis: Converting Feedback Into Insights
Collecting feedback is only half the battle - you must turn it into actionable insights. The right analysis method depends on your resources and timelines.
| Method | Speed | Depth | Scalability |
|---|---|---|---|
| Manual (Interviews/Focus Groups) | Slow; labor-intensive | High; allows for deeper exploration | Low; not suited for large groups |
| Automated (AI/Text Analytics) | Fast; real-time analysis | Moderate to High; identifies patterns across large datasets | High; processes data from multiple channels simultaneously |
Manual analysis, such as interviews or focus groups, offers depth that automated tools might miss. These methods let you explore patient concerns in detail, pick up on non-verbal cues, and address complex emotions. However, they require significant time and aren’t practical for analyzing feedback from large populations.
Automated analysis through AI and Natural Language Processing (NLP) speeds up the process. These tools can sift through call transcripts, chat logs, and social media posts to detect sentiment and trends. They’re especially useful for handling large datasets, spotting patterns that might take weeks to uncover manually.
For the best results, combine both approaches. Use automated tools to identify trends and flag potential issues across your patient base, then dive deeper with manual methods to uncover the reasons behind the data. For instance, if sentiment analysis shows a dip in satisfaction after a specific interaction, follow up with interviews to understand the cause.
Centralizing your data sources and incorporating feedback from frontline staff can also help pinpoint and address systemic issues.
Action: Implementing Changes Based on Feedback
Feedback only makes a difference when it leads to action. Companies that actively respond to patient suggestions experience 41% higher revenue growth.
Real-time responses are especially important for negative feedback. Set up automated alerts to notify staff when patients report poor experiences. This approach, often called "service recovery", can rebuild trust - 75% of patients are willing to forgive mistakes if they feel the organization delivers strong overall experiences.
When addressing negative feedback, follow a clear process: thank the patient, apologize for the issue, offer a solution, and move the conversation to a private channel to protect their privacy. This step is crucial for staying HIPAA-compliant and safeguarding sensitive health information.
For long-term improvements, review feedback regularly to identify recurring themes. These patterns can highlight gaps in processes, confusing communication, or barriers in patient support programs. For example, if patients frequently mention difficulty understanding medication instructions, it might be time to update your educational materials or rethink your delivery methods.
Finally, close the loop by letting patients know about the changes you’ve made based on their feedback. Communicating these improvements shows that their input matters and encourages ongoing participation in your feedback programs. This step not only strengthens trust but also completes the feedback cycle, ensuring a more effective system overall.
Common Challenges in Patient Feedback Collection
Gathering patient feedback comes with its fair share of hurdles. Studies show that many patients hold back from sharing honest opinions, fearing their comments could impact their treatment or upset their healthcare providers. Time is another obstacle - patients with packed schedules often skip providing feedback. Psychological barriers like anxiety, mistrust, and even cultural differences further complicate the process. On top of that, healthcare staff may resist feedback initiatives, either because they worry about criticism or simply don’t have the bandwidth to handle it due to heavy workloads. Another major issue is health literacy. With only about 21% of adults possessing basic health literacy, overly complex feedback forms can discourage participation. These challenges highlight the importance of building trust and simplifying communication to encourage more meaningful feedback.
Building Trust with Patients
Trust is the cornerstone of effective feedback collection. A good starting point is offering anonymity - allow patients to share their thoughts without revealing their identity, which can ease concerns about potential repercussions. Transparency is just as critical; explain how their feedback will be used to improve care. Following through is equally important - show patients the concrete changes made based on their input. As noted in one study:
"Insights into clinical processes and care, based on the lived experience of patients throughout their treatment process, provide a unique and valuable contribution to the prevention of errors and mitigation of risks." – Amelie Koch et al., Institute for Patient Safety
To address health literacy barriers, keep communication simple. Use plain language and incorporate visual aids, like animations, to make information easier to understand. For digital tools, provide brief orientation sessions to help patients who may be unfamiliar with the technology. By building trust and making the process accessible, healthcare providers can encourage more honest and actionable feedback.
Meeting Compliance and Data Security Requirements
Concerns about data privacy can discourage patients from participating in feedback systems. To address this, use HIPAA-compliant tools with strong encryption and secure data storage. Clearly explain what data is being collected, who has access to it, and how it’s safeguarded - this transparency helps build confidence. Implementing standardized protocols for data management, monitoring, and quality assurance is another crucial step in protecting confidentiality and meeting regulatory standards. Online feedback systems should include end-to-end encryption, and a centralized platform can streamline the management of CAHPS (Consumer Assessment of Healthcare Providers and Systems) data. When negative feedback surfaces publicly, respond quickly and move the conversation to a private channel to protect patient privacy. By ensuring data security and compliance, you not only address privacy concerns but also create a feedback system that patients can trust.
Improving Feedback Channels with Patient Mentorship
Patient mentorship programs bring a much-needed personal touch that’s often missing from traditional digital surveys. When seasoned patients guide newcomers through their treatment journeys, they create a trusted bond that encourages open and honest feedback. This approach helps address common barriers like fear of judgment, time constraints, and lack of trust by fostering a safe space where patients feel comfortable sharing their genuine experiences.
These mentorship programs also help uncover insights that might otherwise go unnoticed by researchers and healthcare providers. Nancy Santanello, M.D., M.S., a healthcare consultant, highlights the importance of collaboration in this process:
"Engaging patients, caregivers or organizations... as partners throughout the registry life cycle can help to ensure that the registry effectively collects and measures outcomes that are relevant to patients."
But the benefits don’t stop at better feedback. Mentorship programs also deliver measurable results for businesses. When patients receive personalized guidance, they’re more engaged with their treatment and more willing to provide detailed feedback. This, in turn, gives pharmaceutical and med-tech companies the insights they need to improve their products and services. By blending this human-centered approach with digital feedback tools, companies can unlock actionable insights that drive meaningful change.
How Real-Time Patient Mentorship Works
Real-time mentorship creates an ongoing dialogue between experienced patients and those just starting their treatment journey. Unlike one-time surveys, this continuous support ensures feedback is gathered at multiple stages, helping patients navigate complex healthcare decisions while capturing rich, contextual data about their experiences.
Mentorship transforms the patient-provider relationship into a continuous feedback loop. Through regular check-ins and open-ended conversations, mentors use active listening to help patients voice concerns they might hesitate to share in traditional surveys. This personalized support not only reduces feelings of isolation but also empowers patients to speak openly about challenges like side effects, adherence issues, and quality-of-life impacts that clinical trials might overlook.
Programs like PARTNERS PPRN (Patients, Advocates and Rheumatology Teams Network for Research and Service) illustrate this concept in action. This initiative developed a "key driver diagram" to reduce barriers and boost enrollment in juvenile idiopathic arthritis studies using patient-focused interventions. Similarly, iConquerMS™ tapped into the influence of trusted MS patient bloggers to encourage participation.
The insights gathered through mentorship go far beyond simple survey responses. Instead of collecting ratings or yes/no answers, mentors gather detailed narratives about what’s working and what isn’t. These stories help pharmaceutical and med-tech companies pinpoint specific pain points - from unclear dosing instructions to confusing packaging - that they can address to improve adherence and outcomes. Combining mentorship with data-driven insights enhances this process even further, creating a feedback system that’s both comprehensive and actionable.
Using Sentiment Analytics to Improve Feedback Systems
While mentorship provides in-depth qualitative insights, sentiment analytics adds a powerful layer of quantitative analysis. Natural Language Processing (NLP) tools can sift through thousands of mentorship conversations, transcripts, and chat logs to detect patterns that might escape manual review. Together, these approaches form a feedback system that captures both the "what" and the "why" behind patient experiences.
Sentiment analytics focuses on indirect feedback - such as tone, word choice, and emotional cues in patient communications. Adam Bunker from Qualtrics explains the potential of this technology:
"A robust Voice of the Customer program can do far more than just reveal customer sentiment – the right tools can help you squash reputational risks before they even arise."
This technology allows companies to identify emerging issues before they escalate into public complaints or poor adherence rates. The data supports this: brands that actively respond to feedback see 41% higher revenue growth, and customers are 2.4x more likely to remain loyal to companies that listen and resolve issues quickly. For pharmaceutical and med-tech companies, this means improved patient retention and better treatment outcomes. PatientPartner’s platform exemplifies this dual benefit by combining real-time mentorship with sentiment analytics, offering both the personal touch of human connection and the precision of AI-driven insights.
These insights also help companies refine their feedback systems on a larger scale. By analyzing which questions resonate and which create confusion, they can adjust surveys and communication strategies. Sentiment analytics also identifies the best timing and channels for feedback requests, reducing survey fatigue while boosting response rates. When real-time mentorship and sentiment analytics work together, they create a unified feedback system that strengthens the strategies discussed earlier.
Conclusion: Building Better Patient Feedback Systems
Creating effective patient feedback systems means doing much more than just gathering data. It requires tapping into multiple channels, analyzing insights centrally, and acting quickly. Collect feedback from various touchpoints - like clinical trials, onboarding processes, and digital platforms - to get a full picture of the patient journey. Organizations that actively gather and respond to patient input often experience higher retention rates and more patient recommendations.
To make sense of this feedback, it’s essential to unify diverse data sources. Consolidate survey responses, social media commentary, and operational metrics into a single platform. Tools like AI-powered Natural Language Processing (NLP) can help analyze call transcripts and unsolicited feedback. This integrated "system of action" ensures small issues are addressed before they escalate into larger problems, such as public complaints or reduced treatment adherence.
Real-time mentorship programs can take feedback collection to the next level by fostering ongoing conversations. Experienced patients, acting as mentors, can guide newer patients through treatment decisions, building trust and uncovering insights that traditional surveys might miss. Platforms like PatientPartner combine this mentorship with sentiment analysis, offering both qualitative and quantitative data to drive meaningful improvements in patient care.
To keep these systems effective, avoid leading questions and ensure surveys are designed with the appropriate health literacy in mind. Automate IVR surveys immediately after support calls to reduce agent bias, and always follow up - thank patients for their input and address negative reviews privately. Tying these feedback efforts to financial metrics, such as Customer Lifetime Value (CLV), can also demonstrate their impact on the bottom line.
Patient feedback should be seen as a tool for improving both operations and clinical outcomes. By combining structured data collection with peer mentorship programs, pharmaceutical and med-tech companies can create systems that build trust, enhance treatment adherence, and improve health outcomes throughout the care journey. This commitment to continuous improvement not only benefits patients but also drives operational success and satisfaction.
FAQs
How can healthcare providers encourage patients to give honest feedback?
Patients may hold back from sharing honest feedback due to worries about privacy, fear of repercussions, or skepticism that their opinions will lead to actual improvements. To ease these concerns, healthcare providers should emphasize that patient feedback will remain confidential or anonymous whenever possible. Offering a variety of feedback channels - like digital surveys, secure text messaging, or in-office kiosks - gives patients the freedom to pick a method they feel most at ease with. For older patients, paper forms can be a practical and familiar option.
Establishing trust is equally important. Tools like PatientPartner, which connect patients with experienced mentors, can encourage open dialogue and assure patients that their voices matter. Providers can further build trust by following up with patients to demonstrate how their feedback has been used to make meaningful changes. Combining confidentiality, flexible feedback options, and visible follow-through creates an environment where patients feel secure in sharing their honest thoughts and experiences.
How does AI help in analyzing patient feedback efficiently?
AI has become a game-changer in transforming patient feedback into meaningful insights with impressive speed. By analyzing input from surveys, chatbots, social media, and mentorship platforms, AI leverages natural language processing to detect sentiment, uncover recurring themes, and flag potential safety issues - tasks that would take far longer if done manually.
These AI-driven tools don’t just stop at analysis. They can also rank issues by urgency or frequency, empowering care teams to tackle critical problems as they arise. On top of that, AI systems can connect patient feedback to outcomes, such as treatment adherence, allowing organizations to spot risks early and take preventive action. For pharmaceutical and med-tech companies, this means gaining a dynamic, data-informed perspective on the patient journey, paving the way for quicker improvements and solutions that truly center on patient needs.
How do patient mentorship programs improve the patient feedback process?
Patient mentorship programs build a deeper connection between individuals and healthcare organizations, turning traditional feedback into an ongoing, supportive exchange. By matching patients with seasoned mentors, companies create an environment of trust that encourages open and honest communication. This not only helps patients feel understood but also leads to more meaningful and practical feedback.
Mentors play a key role in breaking down complicated medical jargon, making it easier for patients to share insights that truly reflect their experiences. Since these mentorship interactions happen in real-time, feedback is collected while the experience is still fresh - avoiding delays or forgotten details. This timely and genuine input allows pharmaceutical and med-tech teams to respond more quickly to patient needs, improve treatments, and achieve better results.
Author

Co-Founder and CEO of PatientPartner, a health technology platform that is creating a new type of patient experience for those going through surgery
Related Articles
Stay Ahead in Patient Engagement
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.


