Study: Behavioral Trends in Patient Engagement 2025

Key Takeaways
Study: Behavioral Trends in Patient Engagement 2025
Patient engagement is transforming healthcare, with digital tools, price transparency, and personalized strategies driving better outcomes. Here's what you need to know:
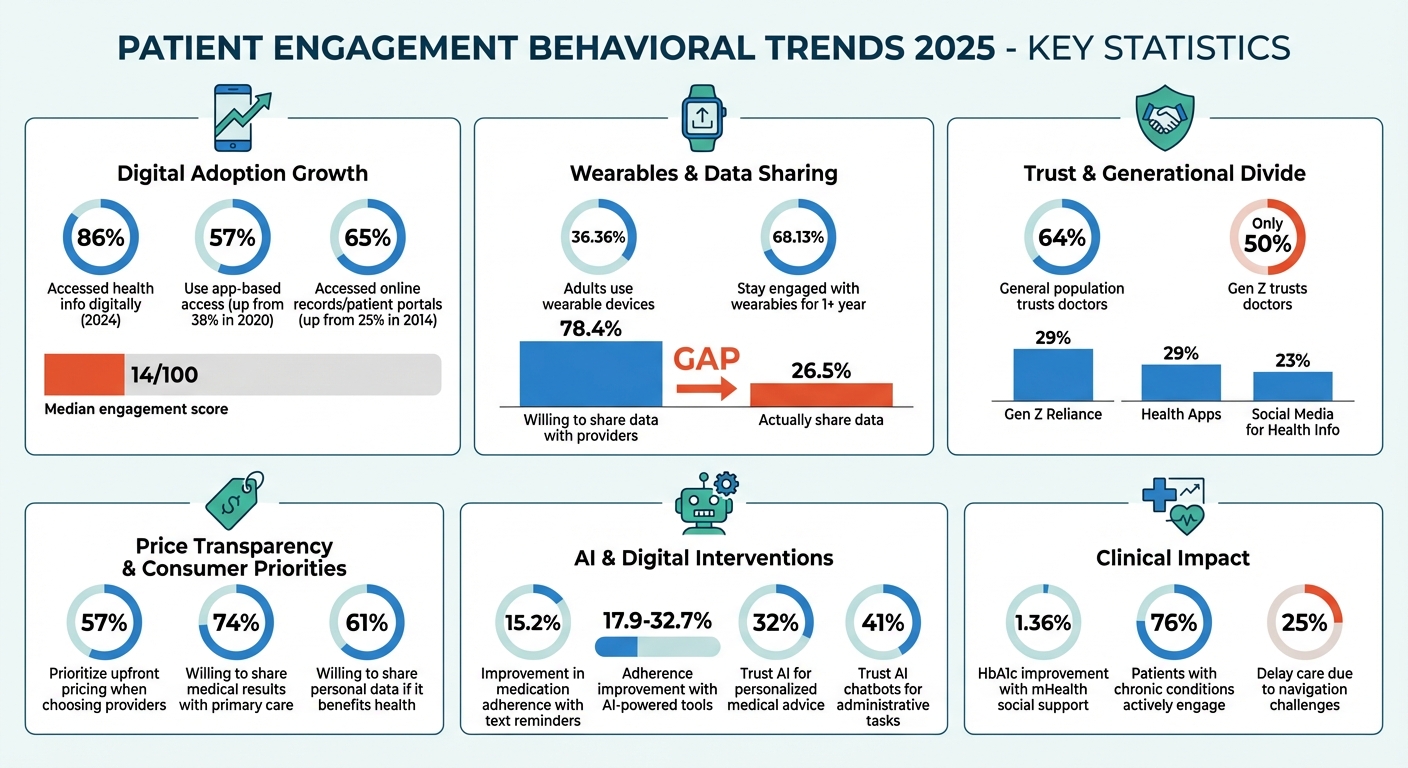
- Digital Usage Growth: By 2024, 86% of patients accessed health information digitally, with app-based access jumping from 38% in 2020 to 57%. However, the median engagement score remains low at 14/100.
- Wearables and Monitoring: Over 36% of adults use wearables, but only 26.5% share data with providers, despite 78.4% being open to it.
- Price Transparency: 57% of consumers prioritize upfront pricing, influencing their choice of care providers.
- Trust Gaps: Only 50% of Gen Z trust doctors, with many turning to health apps and social media for advice.
- AI and Personalization: AI tools improve adherence and simplify healthcare navigation, but trust in AI remains low, especially for clinical tasks.
- Behavioral Nudges: Text reminders boost medication adherence by 15.2%, while tailored AI prompts show even higher effectiveness.
- Social Support: Peer mentorship programs improve outcomes, especially for chronic conditions like diabetes.
- Real-Time Metrics: Tools like the Patient Digital Engagement Index (PDEI) track engagement, linking higher scores to better financial and health outcomes.
These trends highlight the shift toward digital-first, personalized, and transparent healthcare experiences, with a focus on building trust and addressing individual needs.
Patient Engagement Statistics 2025: Digital Adoption, Trust Levels, and Behavioral Trends
Research Scope and Methodology
What Counts as Patient Engagement Behavior
Patient engagement goes far beyond simply showing up for appointments. It includes measurable actions like preparing for visits, following care plans, and refilling medications on time. But it also hinges on less tangible factors like resilience, confidence, and the quality of relationships with healthcare providers - elements that drive these behaviors.
In today’s healthcare landscape, digital engagement plays a central role. The Patient Digital Engagement Index (PDEI) focuses on three key areas: access to care (like online scheduling and managing appointments), financial activity (such as paying bills online or accessing electronic statements), and healthcare information (like using patient portals to view test results).
Study Selection Criteria
The research concentrated on large-scale studies conducted in the U.S. between 2020 and 2025. This period was chosen to capture shifts in patient behavior following the pandemic and the growing role of AI in healthcare delivery. These studies used large, representative samples from across the U.S. to ensure reliable and relevant findings.
Quantitative methods included analyzing electronic health record (EHR) data and using multivariate regression to explore the impact of digital behaviors. The Patient Engagement Capacity Survey (PECS) further supported the research by validating an 18-item tool through exploratory and confirmatory factor analysis. This survey was tested on 1,180 U.S. adults recruited via social media and five ambulatory clinics. Participants were adults who had visited a healthcare provider within the past year.
These methodological choices reflect the unique aspects of the U.S. healthcare system, as discussed below.
U.S. Healthcare Context
The structure of the U.S. healthcare system heavily influenced how engagement was studied. For example, value-based care (VBC) payment models, which reward long-term health outcomes rather than the number of services provided, shaped how digital engagement was tracked and prioritized. Researchers also considered the mix of commercial insurance, Medicare, and Medicaid, as well as federal programs that enhance digital infrastructure at Federally Qualified Health Centers (FQHCs).
Economic factors also play a major role in shaping patient behavior. Over half of consumers (57%) say that cost transparency affects their choice of care providers, making pricing information a critical driver of engagement. Additionally, there’s a noticeable generational divide in trust. While physicians remain the most trusted source of health information overall, only 50% of Gen Z patients trust doctors, compared to 64% of the general population. Younger patients are increasingly turning to health apps and social media for advice instead.
sbb-itb-8f61039
Key Behavioral Trends in Patient Engagement
Digital-First and Multi-Channel Behavior
The way patients engage with healthcare systems has shifted significantly. In 2024, 65% of individuals nationwide accessed their online medical records or patient portals, a sharp increase from just 25% back in 2014. App-based access has also seen a surge, climbing to 57% in 2024, compared to 38% in 2020. Meanwhile, web-only access dropped from 60% to 42% during the same timeframe.
Managing healthcare digitally often means juggling multiple platforms. 59% of patients use several portals across providers, labs, and insurers to piece together their health information. Despite this complexity, digital tools remain popular: 75% of patients believe these tools simplify their interactions with healthcare providers. Features like digital test results (73%), appointment reminders (72%), and self-scheduling (67%) are particularly valued.
Encouragement from healthcare providers plays a key role in adoption. When providers actively recommend patient portals, 87% of patients use them. Without that nudge, the usage rate drops to just 57%.
Proxy access, where individuals manage health records for family members or dependents, is also on the rise. This practice has grown from 24% in 2020 to 51% in 2024. Such trends indicate an increasing openness to digital engagement, setting the stage for broader use of wearables and remote monitoring technologies.
Wearables and Remote Monitoring Adoption
Wearable devices are becoming a cornerstone of patient engagement. By 2022, 36.36% of U.S. adults were using wearables, continuing a steady growth from 30% in 2019. Sustained engagement with these devices is also notable. A study conducted at Cedars-Sinai Medical Center tracked 8,616 patients who linked wearables to their Epic MyChart portal between 2015 and 2022. The findings? 68.13% of patients stayed engaged with their devices for at least a year, with a median engagement period of 21 months.
When it comes to device preferences, Apple HealthKit leads the pack with 83.1% of connections, followed by Fitbit (14.18%), Withings (2.12%), and Google Fit (0.6%). Certain behavioral patterns also stand out. For instance, patients averaging fewer than 5,000 steps per day during their first week of device use were more likely to disengage early. Younger users (ages 18-34) were also more prone to drop off compared to older groups.
Interestingly, there’s a gap between willingness and action. While 78.4% of users are open to sharing wearable data with healthcare providers, only 26.5% actually do so. This suggests that technical hurdles or unclear processes might be holding people back. On the provider side, higher digital engagement has been shown to reduce clinician workloads, challenging concerns that digital tools add to after-hours documentation.
Data Sharing and Trust Factors
Trust plays a pivotal role in how patients approach data sharing. Confidence varies depending on who manages the data. For example, 52% of adults have privacy concerns when hospitals or healthcare providers manage health apps, but this jumps to 78% for government-managed apps and 75% for apps from private tech companies. Despite these concerns, 74% of consumers are willing to share medical results with their primary care providers, and 61% are open to sharing personal data like socioeconomic or behavioral information - provided it directly benefits their health.
Generational differences are striking. While 64% of the general population trusts hospital systems and doctors, this figure drops to 50% among Gen Z respondents. Younger patients are increasingly turning to alternative sources, with 29% relying on health apps and 23% using social media for health information. AI tools face even greater skepticism. Only 32% of the public trusts AI-driven tools for personalized engagement to access medical records, though 41% trust AI chatbots for administrative tasks like scheduling appointments.
Patients managing chronic conditions tend to engage more actively, with 69% participation rates, and those with recent cancer diagnoses reach even higher at 76%. Among older adults with Medicare, 81% prioritize making it easier to securely share health information across providers. However, fewer than 10% of consumers want direct health support from large tech companies, and only 7% currently use apps that consolidate data from multiple sources.
What Drives Adherence and Long-Term Engagement
Digital Reminders and Behavioral Nudges
Text-based nudges have a surprisingly powerful effect on medication adherence. Patients who interact with these reminders - even if only to opt out - reach a 71% adherence rate compared to 55.9% among those who don’t respond, which marks a 15.2% improvement. These prompts also help reduce the median gap in medication refills from 16 days to just 7 days.
However, basic pill reminders often fall short of keeping patients engaged over time. Tailored, interactive prompts are far more effective. For instance, AI-powered tools like facial recognition apps, voice-based conversational AI, and chatbot platforms have shown adherence improvements ranging from 17.9% to over 32.7% across a variety of conditions, including stroke, diabetes, schizophrenia, and breast cancer.
These digital tools work best when integrated into broader support systems, reinforcing long-term adherence.
Social Support and Mentorship Programs
Automated prompts are just one piece of the puzzle - social and peer support programs bring a human touch that’s equally essential. Peer mentorship, in particular, creates a deeper sense of connection that clinical appointments alone often can’t achieve.
Take, for example, a randomized trial at the University of Southern California involving 166 diabetes patients with HbA1c levels of 8.5% or higher. Over six months, participants engaged in a mobile health (mHealth) social support program featuring daily SMS messages to guide supporters. The result? An overall 1.36% improvement in HbA1c levels, with newly diagnosed patients seeing an even greater improvement of 1.96% compared to the control group.
"Partnering with patients, caregivers and community members can advance and optimise the implementation and development of integrated care that is more meaningful for people who use health and social care."
- Kerry Kuluski, Trillium Health Partners
mHealth-based social support eliminates common obstacles like transportation and time constraints, making these programs scalable and accessible. Coordinated efforts, such as sending synchronized messages to both patients and their supporters, ensure timely and relevant assistance throughout the treatment process. Platforms like PatientPartner are already leveraging such models, connecting patients with experienced mentors who provide real-time, personalized guidance, ultimately improving both treatment readiness and adherence.
Personalization and AI-Driven Communication
While digital tools and social support lay the groundwork, personalized AI-driven communication takes engagement to the next level by addressing each patient’s specific needs. For example, about 25% of consumers delay medical care due to challenges in navigating the healthcare system. AI enables tailored communication that simplifies these complexities and tackles the behavioral barriers behind intentional non-adherence.
"AI-powered, personalised approaches are best suited to complex behavioral barriers to intentional adherence."
- Zoe Moon and Jane Walsh, Researchers, Frontiers in Pharmacology
The healthcare industry is increasingly shifting toward "agentic AI", which can handle complex tasks like answering patient questions and managing administrative workflows. This shift is reflected in growing trust: by 2025, only 27% of physicians are expected to view AI as overhyped, down from 40% in 2024. Innovations like ambient listening are already helping reduce administrative burdens, allowing healthcare providers to focus more on patient care.
Personalization also plays a critical role in influencing decision-making. A striking 95% of B2B healthcare buyers say personalized outreach impacts their purchasing decisions. By 2025, it’s estimated that 80% of B2B sales and support interactions in healthcare will occur through digital channels. The most effective strategies blend data insights - like ROI and clinical outcomes - with storytelling that appeals to both the logical and emotional sides of patient decision-making.
Real-Time Metrics and Analytics in Patient Engagement
Core Real-Time Behavioral Metrics
Building on earlier advancements in digital engagement, today's analytics zero in on real-time metrics that turn raw data into meaningful insights on patient decision-making. By 2025, real-time engagement is gauged using the PDEI, now enhanced with data from multimodal telehealth tools. Machine learning models play a key role here, analyzing facial expressions, speech patterns, and text during virtual visits to estimate engagement levels in real time. These models have shown a 40% reduction in root mean square error for engagement estimation compared to older methods. Behavioral cues like hesitation, stress, attentiveness, and emotional states such as anxiety or irritation are some of the key indicators being tracked.
Interestingly, a one-point increase in the PDEI correlates with a one-point rise in patient charges paid over a year. Beyond these metrics, predictive modeling has opened new doors for understanding patient risk profiles.
Predictive Modeling for Risk Identification
Predictive analytics are reshaping how healthcare providers identify and address patient disengagement. By analyzing data from remote monitoring devices and digital interactions, AI tools enable proactive interventions before disengagement occurs. Stephen A. Ferrara, DNP, President of the American Association of Nurse Practitioners, highlights this shift:
"NPs are exploring the capability of AI to analyze vast amounts of patient data from remote monitoring devices to enable proactive interventions."
The results speak volumes. Patients who feel safe in their care report a "Likelihood to Recommend" score of 85.3, compared to just 34.6 for those who don’t offer a top-box response. Similarly, unplanned admissions result in recommendation scores 16% lower than planned ones, underscoring the importance of addressing engagement during critical care moments.
By segmenting patient data based on factors like care journey, race, and age, healthcare providers can pinpoint unmet needs and implement targeted interventions. For example, predictive modeling identifies about 50% of members seeking mental health support as strong candidates for virtual behavioral coaching. With 74% of consumers willing to share personal data to improve their health and an estimated 90 million patients expected to be part of value-based care models by 2027, predictive analytics is becoming a cornerstone for managing large patient populations effectively. These insights also complement real-time sentiment analytics, creating a more refined approach to patient engagement.
Patient Sentiment and Feedback Analytics
Turning patient feedback into actionable strategies is now a critical focus for healthcare organizations. Sentiment analysis tools, used during telehealth sessions, can detect hesitation or stress in real time, allowing providers to adjust their communication strategies on the fly. This real-time approach captures subtle emotional cues that traditional satisfaction surveys often miss.
Higher digital engagement not only benefits patients but also reduces clinician workload. Practices with higher PDEI scores report spending less time on after-hours documentation. Dr. Christopher Apostol of Evans Medical Group emphasizes the importance of patient portals:
"The patient portal is one that we really advocate for because we feel that it is an incredible value for our patients to have access to information, their records, their lab results".
Platforms like PatientPartner are leveraging sentiment analytics to provide real-time insights into patient concerns and challenges. These insights help pharmaceutical and med-tech companies fine-tune their support programs based on real-world patient feedback patterns. These patterns often highlight the impact of mentorship on patient decisions and long-term adherence.
Practical Recommendations for Healthcare Organizations in 2025
Building Programs Around Behavioral Patterns
To make a real impact, healthcare organizations need to go beyond tracking clicks or app usage. The goal should be to measure actual behavior changes - are patients making healthier choices, sticking to treatments, and improving their health outcomes? Technical metrics alone won't tell the full story.
Research from 2021 highlights that patient activation - not just health literacy - plays a key role in improving health outcomes and reducing costs. The Patient Activation Measure (PAM) scores individuals on a scale from 0 to 100, grouping them into four levels of activation. Patients with higher activation levels tend to have better outcomes and lower healthcare costs, even two years after assessment.
Strategies like phased onboarding and team-based care are essential. For example, physicians can focus on meaningful patient interactions, while support staff handle routine tasks. Pre-visit planning, which identifies care gaps before appointments, is another effective approach. Remote patient monitoring (RPM) tools, such as devices that track heart rate and blood pressure, can keep chronic illness management on track by maintaining continuous engagement.
To bridge the digital divide, digital navigators - either specialized staff or peer mentors - can help patients choose and effectively use digital health tools. This kind of human support is critical for keeping patients engaged in real-world scenarios, especially for those with low digital literacy.
Engaging High-Risk Patient Segments
Once robust programs are in place, the next step is to fine-tune them for high-risk groups. This requires digging deeper into data segmentation to identify who might be falling through the cracks. Analyzing data by factors like race, age, and care journey can uncover populations that are struggling with engagement.
For instance, patients who feel safe during care tend to have higher engagement scores. On the other hand, unplanned hospital admissions are linked to a 16% drop in recommendation scores, signaling a critical opportunity for intervention. Older adults, particularly those over 80, and minority groups often report feeling misunderstood or unsafe. Tailored communication strategies and rounding initiatives can address these concerns effectively.
With 76% of adults managing at least one chronic condition, predictive analytics can flag patients at risk of disengagement before it happens. Mental health support is another area where targeted efforts can make a difference - half of those seeking help are ideal candidates for virtual behavioral coaching. To engage diverse communities, organizations should use multilingual tools that reflect cultural nuances. Secure messaging and AI-powered two-way text systems can also help manage the high volume of patient queries, a growing challenge as 68% of physicians report feeling overwhelmed by portal messages in 2025.
Involving Patient and Family Advisory Councils (PFACs) can provide valuable insights into improving communication and program design.
Measurement and Continuous Improvement
Real-time analytics are transforming how healthcare organizations understand patient behavior, but it's essential to go beyond simple usage data. Standardized reporting frameworks that track adherence and emotional engagement are key to driving meaningful improvements. Alarmingly, only 59% of digital health intervention studies currently report even basic usage statistics, leaving a significant gap in understanding.
One critical aspect is identifying the right level of interaction - often called the "target dose" - needed to achieve clinical outcomes. Interestingly, shorter interventions can sometimes be just as effective as longer ones. A review of digital depression interventions found that 9 out of 14 studies showed a direct link between higher engagement and better outcomes.
It's also important to differentiate between patients who drop out due to frustration and those who disengage after successfully reaching their goals. This distinction can help refine program designs and avoid unnecessary interventions for patients who no longer need them.
Workforce engagement plays a major role in patient outcomes. About one-third of healthcare employees report low workplace satisfaction, which can negatively impact patient engagement.
"High workforce engagement strongly correlates with better patient experience and satisfaction."
- Hadly Clark, Director at FasterCures, Milken Institute Health
Improving internal culture and staff satisfaction should be a core part of any patient engagement strategy.
Integrating patient-generated health data (PGHD) directly into electronic health records through APIs allows clinicians to adapt care plans based on real-time behavioral trends. Combining automated data with subjective tools like the Digital Working Alliance Inventory (D-WAI) creates a fuller picture of how patients interact with digital tools. Platforms like PatientPartner use these insights to help pharmaceutical and med-tech companies refine their support programs based on actual patient behavior, rather than assumptions.
Health care technology trends 2025: AI benefits, wearable use cases and telehealth expansion
Conclusion
With 86% of patients using digital tools and 74% willing to share their data, the groundwork for meaningful patient engagement is already in place. However, a median Patient Digital Engagement Index score of just 14 out of 100 highlights a significant gap in how effectively organizations are engaging and supporting patients. These numbers point to a pressing need for more impactful, data-driven strategies to drive better outcomes.
One key factor in improving outcomes is patient activation - the knowledge, skills, and confidence individuals need to manage their own health. Research shows that patient activation is an even stronger predictor of positive outcomes than health literacy alone. Patients with higher activation levels are associated with lower healthcare costs and better health outcomes. By focusing on personalized communication, real-time metrics, and structured support programs, organizations can build patient confidence and see measurable improvements in adherence and overall health.
Peer mentorship platforms, like PatientPartner, offer a way to address trust gaps, particularly for groups like Gen Z, where only 50% report trusting hospital systems. These platforms provide much-needed social support, helping patients navigate complex healthcare decisions and maintain adherence over the long term.
In addition to personalized support, targeted digital interventions can make a real difference. For example, MedStar Health's automated text-message pilot achieved a 28.5% response rate and updated 797 patient records. This demonstrates how streamlined digital tools can directly impact patient care.
Finally, measuring true behavior change - not just surface-level metrics like clicks - is critical. Organizations that combine digital tools with human support, tailor their approaches to patient activation, and refine their strategies using real-time data will be in the best position to improve patient outcomes while driving down costs.
FAQs
How can healthcare providers build patient trust in digital tools and AI?
Healthcare providers can build trust in digital tools and AI by focusing on transparency and privacy. It’s important to clearly outline how patient data is collected, stored, and used, while also showcasing visible security measures. Giving patients access to their own health information - like test results or medication schedules - and letting them decide who can view their data goes a long way in boosting confidence.
Adding a human touch to digital experiences can make a big difference too. For instance, pairing patients with mentors who can guide them through new treatments or technologies brings a personal element to AI-driven tools. Educational resources, such as brief videos or interactive tutorials, can also help patients feel more informed and at ease with these innovations.
Another critical factor is delivering a smooth and dependable user experience. Tools with simple interfaces, consistent performance, and clear benefits are more likely to gain patient acceptance. By regularly gathering feedback and addressing any concerns quickly, healthcare providers can ensure these tools remain effective and trustworthy over time.
What challenges prevent patients from sharing wearable data with their healthcare providers?
Several roadblocks prevent patients from feeling comfortable sharing wearable data with their healthcare providers. Key concerns revolve around privacy and security risks, doubts about whether providers will actually review or use the data, and the lack of smooth integration with electronic health record (EHR) systems. Patients also question the accuracy and usefulness of the data, often believing that providers lack the time or interest to incorporate it into their care plans.
On the flip side, healthcare providers face their own challenges. These include inconsistent data formats, the risk of being overwhelmed by too much information, and uncertainty about reimbursement or liability when using this data. Overcoming these obstacles calls for solutions that build trust, streamline the sharing process, and clearly demonstrate how wearable data can enhance patient outcomes.
Platforms like PatientPartner aim to bridge this gap by connecting patients with mentors who can guide them on securely sharing wearable data. These mentors also help patients understand how this data can be relevant in clinical settings, paving the way for better communication and smoother integration into care routines.
How do real-time metrics help improve patient engagement and health outcomes?
Real-time metrics offer immediate insights into how patients interact with tools like appointment systems, medication reminders, and educational resources. By monitoring actions such as portal logins, completed questionnaires, and adherence patterns as they occur, healthcare providers can quickly spot signs of disengagement and respond proactively. For instance, automated reminders, instructional videos, or live mentor support can help re-engage patients before minor lapses escalate into missed doses or delayed treatments.
These live data streams also enable providers to group patients by risk level, track emerging trends, and align care strategies with broader value-based goals. Studies show that real-time engagement leads to better preventive care participation and improved health outcomes, especially in underserved communities where timely feedback can address gaps in digital literacy. PatientPartner exemplifies this approach by blending real-time mentorship with actionable analytics, enabling pharmaceutical and med-tech companies to enhance patient adherence, increase treatment adoption, and improve overall results.
Author

Patrick Frank, Co-founder & COO of PatientPartner, leads healthcare patient engagement innovation through AI-powered patient support and retention solutions.


