Role of FHIR in Healthcare Data Normalization

Key Takeaways
Role of FHIR in Healthcare Data Normalization
FHIR (Fast Healthcare Interoperability Resources) transforms healthcare data exchange by standardizing how information is shared across systems. Developed by HL7, it uses modern web technologies like RESTful APIs to solve long-standing issues of fragmented and inconsistent patient data. By structuring information into "Resources" such as Patient, Observation, and Medication, FHIR ensures data is accessible, consistent, and interoperable.
Key Takeaways:
- Standardized Data Exchange: FHIR organizes data into modular units, making it easier to share and interpret across systems.
- Semantic Interoperability: Links data to global standards like SNOMED CT, LOINC, and RxNorm for consistent clinical meaning.
- Real-Time APIs: Enables seamless data sharing without complex custom integrations.
- Support for Unstructured Data: Tools like NLP2FHIR help normalize complex clinical notes into usable formats.
- Applications: Drives platforms like PatientPartner, which use normalized data for patient mentorship programs and adherence tracking.
FHIR addresses challenges like inconsistent data formats, unstructured records, and legacy system limitations. Its modular design and use of global standards make it a cornerstone for improving healthcare interoperability, analytics, and patient care.
Getting to Know FHIR: The Best Explanation of FHIR They've Ever Heard
How FHIR Solves Data Normalization Problems
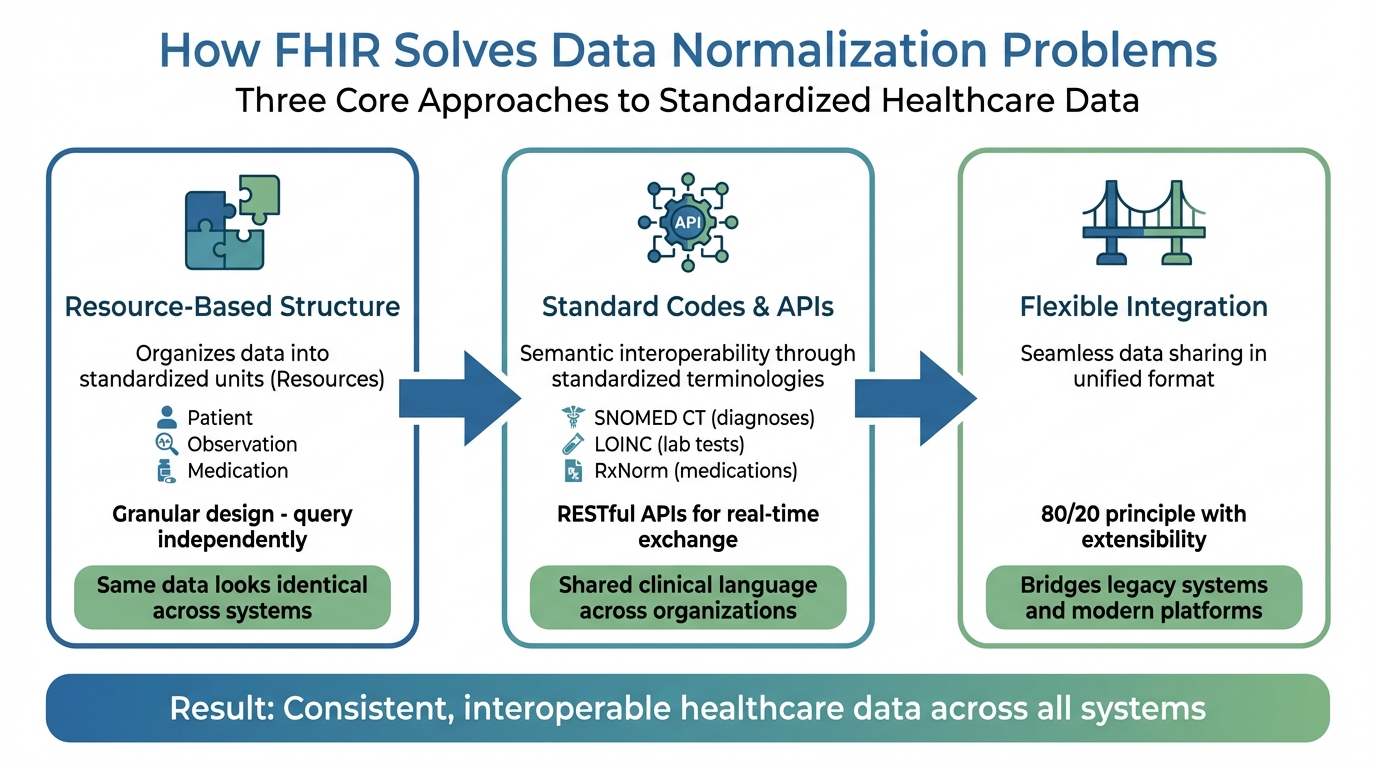
How FHIR Normalizes Healthcare Data: 3-Step Framework
FHIR addresses the challenges of healthcare data normalization using three core approaches: a resource-based structure that organizes data into standardized units, standard terminologies and APIs that ensure consistent data exchange, and flexible integration that allows seamless sharing of information in a unified format. Unlike older, more rigid standards, FHIR's modular design bridges the gap between outdated legacy systems and modern platforms, making data consistency achievable.
FHIR's Resource-Based Structure
FHIR structures healthcare data into standardized units called Resources, such as Patient, Observation, and Medication. Each Resource follows a consistent format that includes common metadata, a human-readable HTML narrative, and structured data elements based on standardized types. This means, for instance, a blood pressure reading recorded in one hospital's system will look and function the same way in another, eliminating discrepancies caused by varying labels for the same data.
What sets FHIR apart is its granular design. Resources can be queried, updated, or exchanged independently, unlike older HL7 v2 segments that bundled data together. For example, a pharmacy system can request only the MedicationStatement Resource without pulling an entire patient record. In more complex situations, FHIR links Resources using references - such as connecting an Observation (like a lab result) to the Patient and Encounter associated with it.
FHIR also supports extensibility. Its base Resources cover the majority of use cases (following the "80/20" principle), but organizations can add custom data elements through extensions without disrupting the core structure. This balance between standardization and adaptability allows FHIR to function effectively across diverse healthcare environments, from small clinics to expansive hospital networks.
Standard Codes and APIs
FHIR achieves semantic interoperability by tying its data elements to standardized terminologies like SNOMED CT for diagnoses, LOINC for lab tests, and RxNorm for medications. This ensures that a diagnosis code recorded in one system has the same clinical meaning in another. By converting local EHR codes into these globally recognized standards, FHIR creates a shared language for healthcare organizations.
The technical foundation of FHIR lies in its RESTful APIs, which use standard HTTP operations like Create, Read, Update, and Search. This web-based approach enables real-time data exchange without the need for custom-built interfaces that were common with older standards. As HealthIT.gov highlights, "FHIR-based application programming interfaces (APIs) have become more prevalent and now offer a new baseline for accessing and exchanging electronic health information nationwide".
For instance, the Mayo Clinic's NLP2FHIR pipeline has shown how even complex clinical narratives can be standardized using FHIR's framework. By leveraging these APIs, applications can ensure reliable data normalization, supporting a wide range of healthcare needs.
Example: PatientPartner Integration
PatientPartner demonstrates how FHIR's normalized data access can drive innovation. The platform helps pharmaceutical and med-tech companies improve patient adoption of new treatments. By utilizing FHIR APIs, PatientPartner retrieves normalized medical history, medication lists, and clinical observations from multiple healthcare systems in a consistent format.
This standardized data supports PatientPartner's mentorship platform, which provides personalized guidance to patients. Using FHIR, the platform automatically pulls data from Condition, MedicationStatement, and Observation Resources through standard queries. This enables its matching algorithm to pair patients with mentors who have relevant experience with similar treatments or conditions.
FHIR's real-time data capabilities also enhance PatientPartner's focus on long-term adherence. As patients move through their treatment plans, clinical data updates automatically, allowing mentors and healthcare teams to quickly spot potential adherence challenges. This data-driven approach, built on FHIR's foundation, enables pharmaceutical companies to monitor patient outcomes and sentiment while staying compliant with healthcare data standards.
Key FHIR Resources for Data Normalization
FHIR structures healthcare data into well-defined, standardized units called Resources. While the framework includes numerous resource types, a study examining nearly 3,000 FHIR profiles revealed that just two - Observation and Extension - make up half of all profiles. These findings highlight their importance when prioritizing implementation efforts.
Patient Resource
The Patient resource is central to FHIR's modular design, offering a standardized foundation for clinical data. It acts as a key reference point for over 69 other FHIR resources. By normalizing essential demographic and personal details - like name, gender, birth date, address, and contact information - it ensures that systems can consistently and accurately identify individuals.
A standout feature is its identifier element, which can store multiple business identifiers such as medical record numbers or Social Security numbers. This capability helps reconcile patient identities across different EHR systems, even when local record numbers differ. Additionally, the resource includes a link element to address duplicate records caused by clerical errors or fragmented data across multiple servers. It uses connection types like "replaced-by" and "replaces" to manage these duplicates effectively.
With a Maturity Level 5 and normative status achieved in FHIR version 4.0.0, the Patient resource is stable and ready for production use. Organizations are encouraged to populate its identifier element with real-world IDs rather than relying solely on FHIR resource IDs, ensuring consistency across systems.
Observation and Encounter Resources
FHIR's clinical data resources, such as Observation and Encounter, play a critical role in maintaining consistency across various healthcare events.
The Observation resource, the most frequently profiled clinical resource with 502 profiles, standardizes data like vital signs, lab results, imaging findings, and social history. It uses a name-value pair structure enriched by metadata, ensuring clarity and uniformity.
On the other hand, the Encounter resource organizes healthcare events by capturing the "who, where, why, and when" of each patient visit. This structure is crucial for tracking a patient’s care over time. For example, linking an Observation to an Encounter allows systems to integrate individual measurements into a larger, longitudinal view of a patient’s health journey.
Both resources strengthen data normalization through terminology bindings. For instance, Observation.code often uses LOINC for lab tests and vital signs, while elements like bodySite rely on SNOMED CT.
Medication Resource
These resources collectively form the backbone of normalized, interoperable healthcare data. The Medication and MedicationStatement resources ensure standardized documentation of prescriptions, drug names, and treatment adherence. By incorporating RxNorm - a standardized drug nomenclature maintained by the National Library of Medicine - they streamline pharmaceutical data management.
For platforms focused on patient adherence, such as PatientPartner's mentorship system, these resources are invaluable. They enable real-time tracking of prescribed medications, treatment initiation, and adherence. By leveraging standardized MedicationStatement data through FHIR APIs, systems can automatically identify patients who may need additional support, connecting them with mentors to improve outcomes.
sbb-itb-8f61039
Benefits of FHIR-Based Data Normalization
By building on the FHIR framework, healthcare organizations can achieve smoother interoperability, sharper analytics, and better patient-centered care.
Better Interoperability and Data Quality
FHIR tackles the challenge of fragmented data head-on. It provides a unified specification for organizing patient information - covering everything from medications to lab results and encounters - ensuring data is consistently understood across systems.
On top of that, FHIR’s RESTful APIs streamline data retrieval and submission. This automation reduces the need for time-consuming manual data mapping, making the process more efficient.
Improved Analytics and AI/ML Applications
Normalized FHIR data lays the groundwork for effective AI and machine learning applications. Its structured and modular format ensures data is ready for analysis without extra validation steps.
Organizations using AI systems integrated with FHIR resources report impressive results, including a 60% reduction in manual document processing. Unlike static snapshots, FHIR APIs enable continuous data flow, unlocking real-time analytics. This capability supports proactive monitoring of patient groups, tracking disease outbreaks, and identifying adverse drug events as they occur.
"Ultimately, FHIR structures the data, while AI makes it intelligent." - Balakrishna Sudabathula, Expert Software Engineer
The healthcare AI market is booming, with forecasts estimating it will reach $188 billion by 2030. Additionally, 84% of healthcare facilities have adopted certified FHIR-enabled API technology, positioning themselves to fully leverage these advancements in analytics.
These breakthroughs in analytics also strengthen platforms focused on patient engagement.
Supporting Patient-Centered Platforms
FHIR's standardized data structure doesn’t just improve analytics - it enhances patient care. By enabling real-time access to clinical information through secure APIs, FHIR supports platforms that prioritize patient needs. For example, when systems consistently process medication adherence data through MedicationStatement resources, they can flag patients who might need extra support.
Take PatientPartner as an example. This platform uses FHIR’s capabilities to connect patients with mentors during critical points in their healthcare journey. By tapping into standardized FHIR data, PatientPartner ensures mentorship interventions happen at just the right moment, boosting adherence rates and improving long-term outcomes.
Additionally, switching from legacy data warehouses to FHIR repositories eliminates the delays caused by overnight batch processing. With this upgrade, patient-centered platforms can quickly adapt to changes in a patient’s clinical status, offering timely, personalized support.
How to Implement FHIR for Data Normalization
Turning the concept of FHIR data normalization into reality requires a well-thought-out plan. Healthcare organizations must adopt clear strategies to convert their existing data into standardized FHIR resources effectively.
Mapping Data to FHIR Structures
The first step is mapping existing data into FHIR resources using tools like FHIR CodeSystem and ValueSet. These tools help retain context and allow for validation. This process involves analyzing both structured and unstructured data to identify equivalent FHIR elements and creating mapping rules that define how each data point translates.
In 2019, researchers at the Mayo Clinic introduced the NLP2FHIR pipeline to standardize unstructured EHR data. Their work validated mapping techniques by achieving F-scores ranging from 0.69 to 0.99 for clinical resource modeling.
"A target data model based on the FHIR type system allows us to easily integrate multiple distinct NLP pipelines, each of which may have their own specialties." - Na Hong et al., Mayo Clinic
A critical part of this process is linking data elements to standard code systems - like SNOMED CT for conditions, LOINC for observations, and RxNorm for medications - to ensure semantic interoperability. Using implementation guides such as the US Core R4 profiles can also help meet U.S. Core Data for Interoperability (USCDI) requirements, improving both data quality and interoperability.
These mapping efforts lay the groundwork for utilizing advanced cloud-based tools for FHIR implementations.
Using Cloud-Based Tools
Cloud platforms make FHIR implementation more manageable by reducing the need for extensive infrastructure. Services like Azure Health Data Services and Google Cloud Healthcare API provide managed environments that handle operations, maintenance, and compliance with standards like HIPAA and ISO, allowing healthcare organizations to focus on data logic instead of infrastructure.
These platforms can ingest data in legacy formats and automatically map it to FHIR, offering high data durability. For example, Google Cloud Healthcare API boasts an impressive 99.999999999% annual durability, ensuring data reliability. Once normalized, FHIR data can be streamed into data warehouses like BigQuery or integrated with machine learning tools such as Vertex AI for deeper insights.
However, it’s important to note that the Azure API for FHIR will be retired on September 30, 2026, with new deployments ending on April 1, 2025. Organizations using this service must plan to migrate to the Azure Health Data Services FHIR service.
These cloud solutions work in tandem with normalization pipelines to create scalable and efficient data transformation systems.
Building Normalization Pipelines
After data mapping and cloud integration, the next step is building robust normalization pipelines. These pipelines should be multi-faceted, combining unstructured text processed through an NLP engine, structured EHR data, and content normalization using the FHIR Composition resource for cohesive document structuring.
In August 2025, a research team led by Alex Bennett and Alistair Johnson demonstrated this approach with the MIMIC-IV Clinical Database Demo on FHIR (version 2.1.0). They converted a 100-patient subset of the MIMIC-IV database into FHIR resources, creating 64 terminology resources and 22 profiles. Custom SQL scripts were used for mapping, and the data was validated on a FHIR server before being exported as compressed NDJSON files for research purposes.
Custom FHIR extensions can also be implemented for additional data points like text offsets and confidence scores. To ensure data integrity, organizations should enable referential integrity in their cloud-based FHIR stores and use resource versioning to track changes over time. Exporting validated resources in NDJSON format not only facilitates analytics but also strengthens interoperability and overall data quality.
Conclusion
FHIR brings together fragmented healthcare data through a standardized, resource-based framework, enabling seamless, real-time exchange across electronic health record systems, medical devices, and healthcare organizations. Its modular design ensures consistency in key data elements while still allowing for tailored extensions to meet specific needs.
Organizations leveraging FHIR-based no-code integration platforms have seen impressive results, cutting data integration timelines by 65% or more and reducing delivery times for complex bi-directional workflows by 80%. The Mayo Clinic's NLP2FHIR pipeline has further highlighted FHIR's ability to standardize both structured and unstructured clinical data effectively.
"FHIR natively aligns with how EHRs exchange data in routine clinical workflows, it offers an opportunity to improve data availability for measurement, enhance alignment between quality measurement and clinical decision support (CDS), and reduce burden." – CMS / HealthIT.gov
Beyond its technical strengths, FHIR supports patient-centered solutions through its API-driven architecture, which enables real-time data access for better care coordination. For instance, PatientPartner (https://patientpartner.com) uses FHIR's capabilities to offer patient mentorship programs that improve treatment adherence and outcomes, aligning with the 21st Century Cures Act requirements.
FAQs
How does FHIR enhance data sharing and interoperability in healthcare?
FHIR improves how healthcare systems work together by providing a web-based API and a standardized data model. This setup allows electronic health records (EHRs), medical devices, and other healthcare systems to exchange information effortlessly. With FHIR, patient data is shared in a consistent, machine-readable format, cutting down on data silos and enhancing care coordination.
By streamlining data standardization, FHIR makes it easier to integrate various healthcare technologies. This not only speeds up data sharing but also ensures its reliability, leading to smarter decisions, better patient care, and a more connected healthcare network.
How do standard terminologies like SNOMED CT and LOINC support FHIR in healthcare data exchange?
Standard terminologies like SNOMED CT and LOINC play a key role in FHIR by offering the structured code systems that define its data elements. These terminologies ensure clinical concepts are represented consistently, which is crucial for accurate data exchange and interpretation across healthcare systems.
By relying on these widely accepted standards, FHIR helps create smooth interoperability between systems. This leads to clearer communication, enhanced patient care, and more efficient data sharing throughout the healthcare landscape.
What steps can healthcare organizations take to use FHIR for data normalization?
Healthcare organizations can use FHIR to streamline data normalization by starting with a thorough review of their clinical data sources. This includes both structured data (like lab results and prescriptions) and unstructured data (such as free-text clinical notes). These diverse data types are then aligned with FHIR resources - like Patient, Observation, or MedicationStatement - using implementation guides that define how to format and standardize the data for interoperability.
Once the data is mapped, the next step is building a data pipeline to handle extraction, transformation, and loading (ETL). This pipeline feeds the information into a centralized FHIR server or repository. The process often relies on automation tools for mapping, validation checks to ensure data accuracy, and batch processing for handling large volumes of data efficiently. To meet specific needs, organizations can also create custom profiles or extensions while adhering to FHIR guidelines.
After normalization, the standardized data can be accessed through FHIR-based APIs. This enables seamless integration with tools like patient portals, analytics platforms, and clinical decision support systems. To maintain reliability, organizations should establish governance practices - such as monitoring API performance and updating standards - to keep the data accurate, secure, and ready for evolving interoperability requirements.
Author

Co-Founder and CEO of PatientPartner, a health technology platform that is creating a new type of patient experience for those going through surgery


