Checklist for Consent Training Programs

Key Takeaways
Checklist for Consent Training Programs
Informed consent is more than a signature - it's a process of clear communication that ensures patient understanding and safety. But studies show many healthcare providers fall short in meeting all required elements. This gap can lead to risks like medical errors, poor patient outcomes, and legal issues.
Here’s how to fix it: A well-structured consent training program. By focusing on clear communication, plain language, and proper documentation, you can improve patient trust and meet regulatory standards.
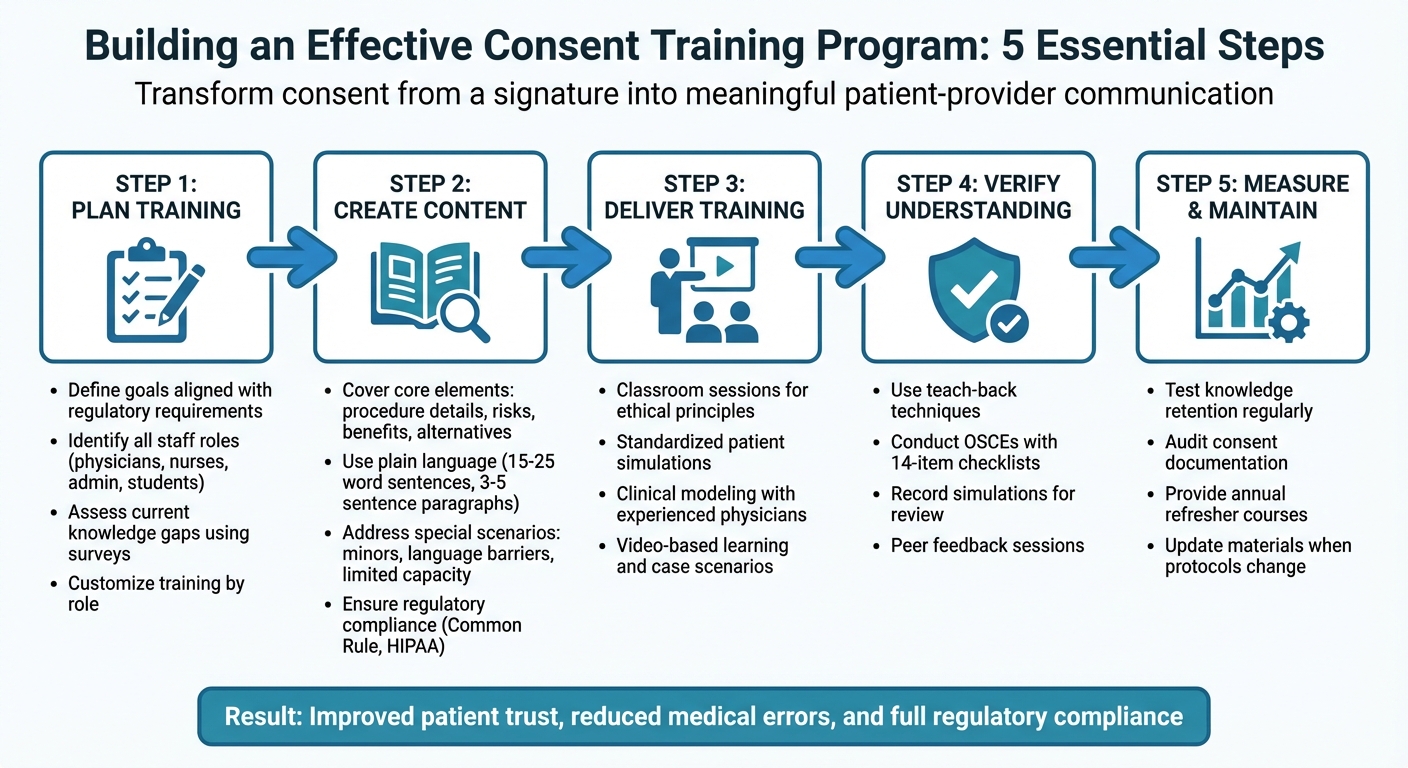
Key Steps:
- Plan Training: Define goals, assess staff knowledge, and tailor training to roles (e.g., surgeons vs. admin staff).
- Core Content: Cover procedure details, risks, benefits, and alternatives upfront in simple language.
- Interactive Methods: Use mock scenarios, teach-back techniques, and video reviews for hands-on learning.
- Special Cases: Train for minors, language barriers, and patients with limited decision-making capacity.
- Measure Success: Test retention, audit compliance, and provide ongoing support like refreshers and updates.
This approach turns consent from a task into a meaningful patient-provider conversation, while ensuring compliance with legal and ethical standards.
5-Step Framework for Implementing Effective Consent Training Programs in Healthcare
Informed Consent - what is informed consent // informed consent training
sbb-itb-8f61039
Planning Your Consent Training Program
When it comes to creating an effective informed consent process, the first step is thoughtful planning. Start by clearly defining what success looks like for your training program. This means aligning your training goals with both regulatory requirements and real-world communication needs. For example, your training should ensure that staff fully understand the essential elements of informed consent, such as the purpose of the research, potential risks, possible benefits, and available alternatives. A key objective is teaching staff to communicate this information using plain language and straightforward sentences to make it easier for participants to understand.
Next, identify everyone who needs training. This could include physicians, nurses, administrative staff, students, and leadership. The Office for Civil Rights emphasizes:
"The HIPAA Rules are flexible and scalable to accommodate the enormous range in types and sizes of entities that must comply with them. This means that there is no single standardized program that could appropriately train employees of all entities"
. This flexibility means you should customize training to fit each role. For instance, a surgeon may require a deeper understanding of risk communication, while front-desk staff might focus on accurately handling consent forms.
Before diving into training, assess your team's current knowledge. Use pre-training surveys or checklists to pinpoint gaps. For example, you could evaluate whether staff can clearly explain risk disclosures or properly document consent using IRB-approved forms. Practical exercises, like reviewing consent forms for readability or participating in mock scenarios, can also help. Research on tools like the MacCAT-T assessment has shown reliable results in measuring skills like understanding information and reasoning about risks and benefits. Additionally, your learning management system can help you establish a baseline and track progress over time.
| Assessment Category | Evaluation Focus |
|---|---|
| Information Sharing | Ability to explain procedures, benefits, risks, and alternatives |
| Communication | Use of clear, jargon-free language while maintaining rapport |
| Verification | Effectiveness in using "teach-back" methods to confirm understanding |
| Documentation | Proper use of IRB-approved forms and obtaining necessary signatures |
Creating Training Content
Once your program is planned, the next step is crafting clear and practical training materials that comply with regulatory standards.
Core Elements of Informed Consent
Your training materials should thoroughly cover the essential aspects required for valid and ethical consent. Start with the basics: include a clear statement that the study involves research, its purpose, duration, a detailed description of all procedures (highlighting which are experimental), potential risks or discomforts, anticipated benefits, and available alternatives. According to the Revised Common Rule, consent must begin with a "concise and focused presentation" of key information to help individuals decide whether to participate. Make sure this key information is presented upfront.
As the MRCT Center explains:
"Consent forms are not transactional documents like other contracts – they are tools to help facilitate an informed choice".
Your materials should also emphasize that participation is voluntary, refusal carries no penalty, and participants can withdraw at any time. Additionally, address practical details such as confidentiality measures, any costs to participants, and conditions under which an investigator might end their participation.
Health literacy plays a critical role. Train your team to draft consent forms using plain language - short sentences (15–25 words), concise paragraphs (3–5 sentences), and a minimum 12-point font. Encourage active verbs (e.g., "collect" instead of "collection") and use headings phrased as questions - like "What are the risks?" - to guide readers effectively.
Finally, ensure your training addresses unique challenges in special consent scenarios.
Special Consent Situations
Not all consent situations are straightforward, so your training must prepare staff for more complex cases. For example, when working with minors, the process requires "informed permission" from parents for children under 17, while the child provides "assent", except in cases of legally emancipated adolescents. Make these distinctions clear in your training.
Language barriers present another challenge. Emphasize the importance of using qualified interpreters rather than relying on family members, and ensure consent forms are available in the patient’s primary language. Include training on cultural competency to help staff navigate cultural or disability-related barriers. For patients with limited decision-making capacity, outline protocols for assessing competency and clarify when a legally authorized representative (LAR) is needed. The "reasonable patient standard" should guide staff to provide the average patient with the essential information needed for an informed choice.
Your training should also cover proper documentation for various scenarios. For example, explain when to use a full written consent form versus a "short form" for oral presentations, which requires a witness and a written summary. Additionally, clarify the criteria under which an IRB may waive the need for a signed consent form.
Once the materials are developed, focus on interactive methods to ensure staff fully understand and apply the concepts.
Interactive Learning Methods
Lectures alone won’t cut it. Instead, incorporate hands-on approaches like standardized patient exercises, which are highly effective for both teaching and assessing performance. These simulations allow staff to practice the full consent process in a controlled setting with trained actors.
Simulation exercises can reinforce consent communication skills. For example, APGO’s module demonstrated the value of using checklists to assess these skills.
Video-based learning is another powerful tool. Recordings of expert clinicians modeling effective consent techniques or videos of learners’ performances can be used for group or individual review. These methods encourage self-reflection and peer feedback. Detailed case scenarios can also help learners combine medical knowledge with strong communication skills. If the focus is on evaluating communication, consider providing procedure fact sheets before simulations.
Structured assessments are equally important. Use Objective Structured Clinical Examinations (OSCEs) at the end of clinical rotations to formally evaluate and reinforce informed consent skills. Peer mentorship programs can further boost engagement and provide ongoing support for skill improvement. Finally, conduct usability testing with target users to fine-tune your materials before final implementation.
Delivering the Training
The way you deliver training can significantly impact how well your staff retains information and applies it in practice, much like mentorship’s impact on patient decision making. Choices about training formats, methods to confirm understanding, and strategies to address challenges are all key to ensuring your consent training program succeeds.
Choose Effective Training Formats
Start with classroom sessions to introduce ethical principles and basic communication skills. As learners progress, move into simulated settings using standardized patient exercises, an approach endorsed by APGO. These simulations provide a safe space for learners to practice and refine their skills.
Clinical modeling is another critical component. Watching experienced physicians conduct informed consent discussions during clinical rotations helps reinforce learning. For instances where direct clinical exposure is limited, video-based learning can fill the gap. If your training focuses more on communication skills than medical knowledge, consider providing procedure fact sheets ahead of simulations. This allows learners to concentrate on interaction techniques without being distracted by unfamiliar medical details.
By combining these formats, you create a well-rounded, practical learning experience.
Incorporate Teach-Back Techniques
After selecting your training formats, it’s essential to ensure learners truly understand the material. One effective method is teach-back, which not only verifies patient comprehension but also evaluates how well providers communicate. Train staff to ask patients to verbally summarize the information shared with them. As APGO explains:
"Informed consent is a process of information sharing that allows patients to make informed choices, not simply a signature on a form."
During standardized patient exercises, use checklists to guide the teach-back process. Staff should be able to clearly explain the procedure - covering indications, benefits, risks, alternatives (including opting out), and post-procedure expectations - and verify that patients can repeat this information back accurately.
Address Common Challenges
Integrating consent training early in a professional’s career can help mitigate challenges like staff turnover and limited time for clinical exposure.
When time constraints limit hands-on practice, use video tools, standardized patient simulations, and checklists to ensure all core elements are consistently covered. For staff who view consent as just a signature rather than an ongoing exchange of information, group video reviews can shift this mindset. Watching and discussing recorded consent interactions promotes peer learning and helps refine communication skills. This approach turns time limitations into opportunities for growth, ensuring staff continue to improve their ability to navigate the consent process effectively.
Measuring and Maintaining Training Programs
Once training is delivered, the real work begins - ensuring that knowledge sticks and is applied consistently. This involves measuring retention, monitoring compliance, and providing ongoing support. These steps complete the training cycle, bridging the gap between learning and real-world practice.
Test Knowledge Retention
In 2017, the Association of Professors of Gynecology and Obstetrics (APGO) introduced a performance assessment framework that uses a 14-item checklist during Objective Structured Clinical Examinations (OSCE). This checklist evaluates specific actions, like whether the provider "Offers alternatives for the procedure, including no intervention" and "Verifies patient understanding." These assessments, conducted at the end of rotations, help confirm whether learners are truly prepared.
Simulations can also be recorded for self-review or group feedback, providing opportunities to evaluate verbal explanations and non-verbal communication. Another effective method is the teach-back technique, where providers ask patients to repeat information in their own words. This approach directly measures how well communication skills have been absorbed and ensures that patients understand the information being shared.
Once retention is validated, the focus shifts to how well these skills are being incorporated into daily workflows.
Monitor Compliance and Results
Regularly track metrics and audit consent documents to ensure they meet regulatory standards and use clear, accessible language. Compliance checks should align with regulations like the Common Rule (§46.116), helping to identify and address issues before they become significant problems.
Peer benchmarking is another valuable tool. Comparing your organization’s performance against similar institutions can highlight strengths and pinpoint areas needing improvement. Many organizations now leverage AI and machine learning to analyze documentation patterns, flagging potential risks before they escalate. The Joint Commission emphasizes the importance of such evaluations:
"Evaluation findings provide useful feedback that informs program developers of refinements that may be needed to better assist organizations with their improvement efforts and help inform decisions about future initiatives or strategic priorities."
Provide Continued Support
Ongoing support is key to maintaining high standards. Annual refresher courses help reinforce consent practices, while video reviews of consent discussions offer valuable insights for individual or group learning.
Whenever protocols change or new treatments are introduced, updated procedure fact sheets should be distributed to ensure providers have the latest information. Establishing a system to share organizational strengths as "leading practices" across departments can further enhance consistency and improve outcomes across the board.
Conclusion
Improving consent training can transform how healthcare providers communicate with patients. Using a structured checklist ensures that every critical element is addressed - covering everything from the nature of procedures to potential risks, benefits, and available alternatives. Studies reveal notable gaps in current practices, emphasizing the importance of adopting a more systematic approach.
Moving away from a process that prioritizes signatures to one that focuses on meaningful communication reshapes the way informed consent is handled. This approach highlights that informed consent is about far more than just obtaining a signature - it’s about fostering understanding. This shift in perspective should inform every step of your training program, from initial development to regular evaluations, creating a foundation for a checklist that captures all essential elements.
As outlined earlier, a well-organized checklist not only aligns training with established best practices but also supports compliance with federal regulations. More importantly, it improves patient outcomes. Incorporating tools such as the teach-back method ensures that patients feel comfortable asking questions, while providers communicate more clearly. This approach protects patient autonomy and strengthens organizational adherence to legal standards.
To maintain success, regular evaluations, peer comparisons, and continuous improvements are key. Treating informed consent as an ongoing conversation, rather than a one-time task, helps healthcare providers respect patients’ rights to make choices that reflect their personal values and preferences.
FAQs
How can healthcare providers help patients fully understand informed consent?
Healthcare providers can make sure patients truly understand informed consent by approaching it as an open, two-way conversation instead of a mere formality. Start by considering the patient’s unique needs - this might include their level of health literacy, language preferences, cultural background, or familiarity with the procedure or condition. Tailor the discussion to cover essential points like risks, benefits, alternatives, and what the process entails.
Use clear, everyday language, steering clear of medical jargon. Break down complex ideas into smaller, more digestible parts, and back up verbal explanations with tools like written handouts, visual aids, or diagrams. To ensure comprehension, try the teach-back method: ask patients to repeat the key points in their own words. This helps confirm they’ve grasped the information. Be sure to encourage questions, allow time for thoughtful reflection, and document their understanding.
For additional support, healthcare providers can team up with PatientPartner, a resource that connects patients with mentors who can reinforce consent details, address lingering concerns, and help patients stick to their care plans over the long term.
How can consent training programs address language barriers effectively?
Language barriers can make it challenging for patients to fully grasp consent information, potentially jeopardizing both their safety and regulatory compliance. To tackle this issue, consent training programs need to focus on practical ways to close communication gaps.
Here are some effective strategies:
- Rely on certified medical interpreters during consent discussions, rather than depending on family members or untrained staff, to ensure accuracy and professionalism.
- Use professionally translated consent forms and materials in the patient’s primary language. These should be clear and culturally sensitive to avoid misunderstandings.
- Train staff to work effectively with interpreter services and confirm patient understanding through methods like the teach-back technique.
By integrating these approaches into training, healthcare providers can build trust, minimize errors, and ensure fair and comprehensive care for patients with limited English proficiency.
What are the best ways to measure the success of a consent training program?
To measure how effective a consent training program is, organizations can rely on a mix of quantifiable metrics and participant feedback. This can include evaluating knowledge retention through quizzes or assessments, monitoring shifts in workplace behavior, and collecting input from participants about their training experience.
Another useful approach is applying the Kirkpatrick model, which breaks evaluation into four levels: participant reaction, what they learned, how their behavior changes, and the program's overall influence on organizational goals. This framework offers a thorough way to gauge whether the training achieves its intended outcomes and drives better workplace practices.
Author

Lidia Chesnokova, VP of Client Success at PatientPartner, drives patient engagement software strategy and personalized support solutions in healthcare.


